NURSE COMPETENCIES

ILD Nurse Competencies
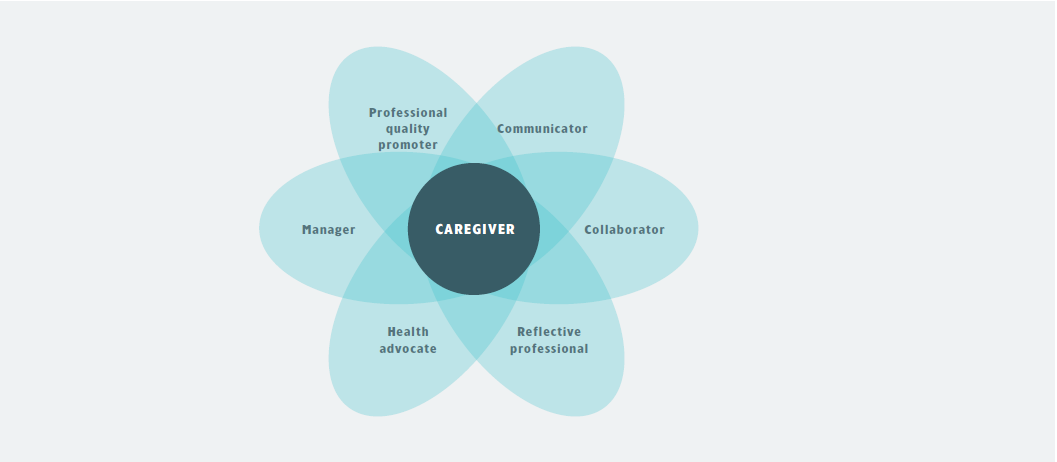
Nurses play a central role in providing healthcare and are especially valued by patients with complex diseases, such as interstitial lung disease (ILD). Due to the growing complexity of care, the roles of specialist nurses is evolving in ILD. To provide and coordinate optimal holistic care that is tailored to the patient’s individual needs and values, they have several roles for which they need certain competencies.1 These roles and competencies are depicted by the framework below.
|
Adapted from the CanMEDS-model developed by the Royal College.2
CANMEDS-MODEL
CanMEDS (Canadian Medical Education Directions for Specialists) is a framework that was originally created to define the competencies that physicians need to ensure good practice.2 This framework was later adapted by a Dutch workgroup to describe the competencies that nurses require to meet the needs of patients. Since then, a new variant of the framework was developed by ILD specialist nurses for optimal ILD nursing.
The CanMEDS model described here, displays the abilities for ILD nurses to ensure optimal ILD care. For every CanMEDS-role, the nurse should possess certain competencies that consist of knowledge and skills.
CENTRAL ROLE: CAREGIVER
The nurse as a caregiver is the central role to which the other roles are connected. ILD nurses have broad knowledge ranging from disease specifics to how to deliver care. Their close relationship to the patient allows them to recognize individual needs and provide holistic care that may include the provision of therapeutic interventions, information, advice and support. ILD nurses combine information from the patient’s physical, psychological, functional and social functioning and know how to strengthen the self-management of patients to cope with their disease.
Executive roles
General
- Main point of contact for patients’ and caregivers’ concerns and questions
- Educate patients about aspects involving ILD (pathogenesis, symptoms, diagnostics and treatments) and lifestyle changes to improve disease course
- Assess care needs, make care plans and finally implement the care plan
- Give advice to strengthen self-management or refer to additional healthcare providers or support groups
Monitoring
- Follow-up of patients after diagnosis
- Clinical evaluation to detect changes in health status (e.g. ILD progression, comorbidities or impact and side effects of treatment)
- Measuring oxygen saturation
- Assessing exercise capacity
- Weight
- Psychological status
Treatment monitoring
- Immunomodulatory or anti-fibrotic therapy
- Management of side effects
- Non-pharmacological treatment
- Supplemental oxygen
- Pulmonary rehabilitation
- Supportive care/Palliative care (e.g. symptom relief, psychosocial support)
- Nutritional advice
Knowledge
- Is familiar with the principles of clinical reasoning and nursing
- Knows the basic principles of the pathogenesis, symptoms, diagnostics and treatment of ILD
- Can interpret test results and recognize symptoms
- Recognizes signs that warrant evaluation by a pulmonologist/other physician
- Is familiar with protocols and guidelines concerning ILD
- Knows management strategies for ILD and the impact of treatments
- Knows how to provide and manage treatments
- Has an understanding of the physiological aspects related to ILD
- Knows the impact of ILD on the patient’s life and knows how to improve his/her quality of life or prevent deterioration
- Understands the impact of exercise and lifestyle on ILD and knows how to motivate patients
- Is aware of where patients and caregivers can go for help and information, such as patient associations and homecare providers
Skills
- Can collect and interpret information from the patient and set up goals together with the patient
- Extracts the core, patterns and connections from a relatively complex or large amount of data
- Is able to determine the need for support through clinical reasoning
- Can give education about how to reduce breathlessness and improve overall health
- Is able to monitor progress and evaluate results of interventions on the patient’s physical, psychological, functional and social well-being
- Recognizes changes in the health of the patient
- Structures and plans actions according to available time and resources, and takes into account priorities when processing information and tackling problems
- Follows generally accepted social and ethical standards, acts consistently according to them and shows integrity and reliability
- Shows stress resistance; continues to function efficiently in difficult situations, under strong pressure, in the event of errors and/or criticism
- Shows empathy and takes into account feelings, needs and wishes of the patient and his/her caregiver
Communicator
A diagnosis of ILD can impact the daily lives of patients and their families in many ways. Effective communication is essential to help patients cope with their disease in the best possible way.3 Clear information that is tailored to the patient’s preferences and needs may help the patient to retain control and make well-informed decisions. Effective communication also allows to get a thorough understanding of the patient’s fears and worries, which makes the patient feel understood and supported.
Nurses are trained in communication skills that allows them to discuss prognosis, goals of care, advance care planning options, and medical decisions with the patients and caregivers. They can facilitate sensitive conversations in a supportive manner and consider the patient’s concerns and values in making decisions.4 Although nurses may not agree with the patient’s ideas, it is essential for them to accept the patient’s views and values, and give him/her space for reflection.
Non-verbal language is the fundamental basis of communication. What is said is as important as how things are said. As such, posture, facial expression and tone of voice are fundamental aspects of communication.
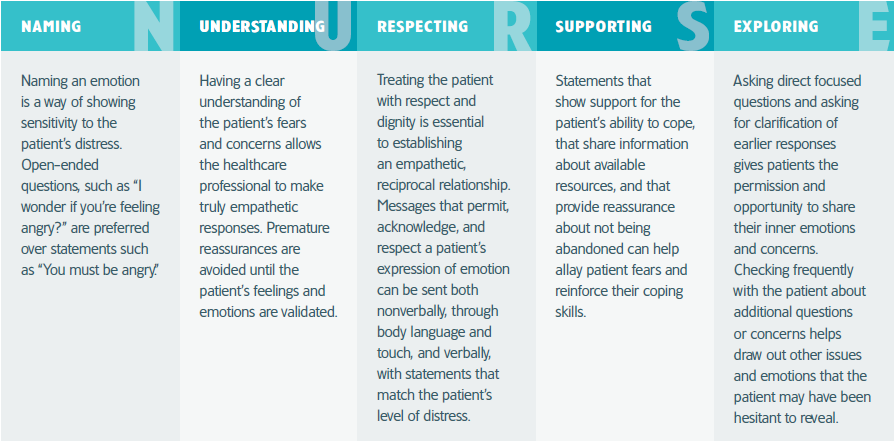
Supporting the patient in a constructive and empathetic manner may be difficult. A strategic plan may help to provide clear information in a supportive manner. There are various strategies or protocols designed to describe how to carry out difficult conversations or respond to emotional distress. Among these are the SPIKES protocol, linked here, and the NURSE approach, detailed on the next page5:
Knowledge
- Knows basic principles of effective communication
- Knows what aspects to discuss with patients
- Knows techniques and strategies to carry out conversations and support patients and caregivers
- Is up-to-date with supportive tools to provide information or carry out conversations
Skills
- Is willing and able to correctly record, process and respond to (non-)verbal messages; conveys information in a structured manner (orally and in writing).
- Is able to tailor information to individual patients, based on their background and preferences for information
- Knows how to transform complex information to clear and easy to understand language
- Has courage to initiate difficult conversations
- Knows how to deal with emotional distress of patients and caregivers
- Can show empathy and support in conversations
- Knows when to listen, ask questions or motivate, but also when to manage moments of silence. Deliberate silence can give the opportunity to think and process what comes next in the conversation or to broach a new topic
NURSE
A helpful strategy for responding to patients’ emotional distress with empathy is called NURSE.5
|
Collaborator
ILD nurses act as a link between healthcare providers and patients and their family.6 Due to their personal relationship with the patient and availability, they are the first and main contact for patients and their caregivers. This allows them to assist and support patients to improve their self-management, and transfer relevant information to healthcare providers of other disciplines. They must therefore understand the needs of other healthcare providers and provide expert advice as a consultant. As part of a multidisciplinary team, ILD nurses cooperate with other healthcare providers to provide care that is responsive to the patient’s needs and values. As such, ILD nurses act as coordinators to ensure continuity of care for the individual patient.
Knowledge
- Is familiar with concepts of collaboration and knows how to facilitate effective collaboration
- Has knowledge of different ethnic, cultural and religious backgrounds that patients may have
- Has knowledge of the patient’s family and social environment
- Knows about management strategies for ILD and how ILD care is organised
- Knows potential collaborators within ILD care and is able to refer to appropriate healthcare providers
- Is familiar with appropriate methods for reporting and sharing of information
- Is able to provide appropriate advice as a consultant to other healthcare providers
Skills
- Has good communication skills
- Shows empathy and respect for the patient’s values, beliefs and preferences
- Is able to take on a coordinating role, switching from collaboration with different healthcare providers to collaboration with patients and caregivers
- Is able to formulate conclusions and action points from (multidisciplinary) meetings to solve problems or conflicts and facilitate a smooth-running care process
- Knows how to clearly communicate the responsibilities of professionals within the ILD team and oversees the tasks are taken care of
Reflective professional
To improve ILD care, nurses should reflect the current practices within their ILD team and strive to improve this. Nurses could increase their knowledge through experience, case discussions, peer assessments and education. They aim to develop their expertise and contribute to the expertise of other ILD nurses to obtain general high standards of care. For this, they know how to set objectives for members of the care team and ensure that these are met in a realistic time frame. They know how to keep an eye on the learning objectives and practice of themselves and colleagues, and take on a mentoring role to support others in improving their knowledge and skills.
Knowledge
- Knows the current practices of other ILD expertise centres to reflect on their own organisation
- Knows the latest insights in ILD care
- Optimizes one’s own knowledge of the area of expertise (evidence based practice) by means of scientific literature, self-study, following training courses or attending symposia
Skills
- Is able to network and collaborate between ILD nurses and other ILD experts
- Can critically look at own practices and formulate ways to improve this
- Is eager to develop as a professional
- Has an eye for learning objectives and processes of colleagues and provide them with appropriate support
- Implements clinical developments in the practice of the healthcare providers, and thus increases the level of expertise of the team
- Deals with feedback in a constructive way, and takes actions to promote his/her professional and personal development
Health advocate
ILD nurses help to improve the health of patients by supporting them to eat healthy, exercise and adopt self-management strategies. They can educate patients about how to improve their health or refer to appropriate resources and healthcare providers for additional support. ILD nurses also watch over the quality and continuity of care and advocate for patients’ and caregivers’ preferences in multidisciplinary discussions.
Knowledge
- Has an understanding of the physiological aspects related to ILD
- Understands what factors are known to improve the course of ILD
- Knows how to clearly educate about ILD-specific symptoms and ways to reduce them
- Familiar with ways to encourage a healthy lifestyle
Skills
- Is able to provide individualized support based on patient’s symptoms, needs and values
- Can transform complex information to simple, easy to understand language
- Provides structured education and consultations to patients and their loved ones to promote health behavior, diagnosis and the associated care processes.
Organiser
ILD nurses assess patients’ needs for care, monitor symptoms and disease progression, and come with solutions to meet needs for care. They organise and coordinate various sectors of healthcare while prioritising the interests of the patient and their caregiver.
Knowledge
- Knows appropriate resources for managing symptoms of ILD
- Can influence the policies and organization of the center
Skills
- Is able to make decisions about policy and resources for care based on the individual needs and opinion of different experts
- Is assertive and takes action to ensure optimal care
- Can show leadership
Professional and quality promotor
ILD nurses have a responsible and professional attitude to ensure optimal care for ILD patients. They know how to provide care according to the latest insights and guidelines, how to monitor patients for ILD progression and which management strategies are appropriate. With their knowledge and close relationship to the patient, they are able to identify gaps in standards and protocols and are committed to bring this to the attention of their ILD team and colleagues. They can encourage the initiation of scientific research regarding unmet needs, and participates in research and quality projects concerning the specialist nursing domain. When new scientific evidence is available, they know how to incorporate this information in their daily practice. To achieve optimal care, they should be motivated to improve their own skills and practice and spread their knowledge to colleagues and/or patients (e.g. by the organization of educational courses or creation of educational material).
Knowledge
- Knows the current ILD guidelines and protocols
- Is up-to-date with developments in ILD or nursing care; is aware of ongoing research and/or is able to play a role in that
- Can provide knowledge about ILD to other colleagues
Skills
- Is committed to provide optimal ILD care
- Is critical to current practices
- Is enthusiastic to make a proactive contribution to improve quality of care
- Can organize educational courses for healthcare providers and/or patients and participates in theoretical and practical education/training for colleagues
- Actively contributes to the development and implementation of evidence-based protocols and procedures in the clinical domain concerned
Conclusion
In the last couple of years, holistic care has become the standard for providing ILD care. As such, nurses need to adopt many roles for which they need specific knowledge and skills. The CanMEDS-model for ILD care summarizes all these specific competencies in one single framework. To ensure optimal care for ILD patients, it is important that nurses are aware of their own strengths and limitations, develop necessary competencies during their education and career, and support each other to provide the best care possible.
Refrences
REFERENCES
-
Russell AM, Olive S, Lines S, et al. Contemporary challenges for specialist nursing in interstitial lung disease. Breathe (Sheff). 2018;14(1):36-41.
-
CanMEDS. Royal College. Available at. https://www.royalcollege.ca/rcsite/canmeds-e
-
Bernacki RE, Block SD. Communication about serious illness care goals: a review and synthesis of best practices. JAMA Intern Med. 2014;174(12):1994-2003.
-
Hagan TL, Xu J, Lopez RP, et al. Nursing’s role in leading palliative care: A call to action. Nurse Educ Today. 2018;61:216-9.
-
Kaplan M. SPIKES: a framework for breaking bad news to patients with cancer. Clin J Oncol Nurs. 2010;14(4):514-6.
-
Sekse RJT, Hunskår I, Ellingsen S. The nurse’s role in palliative care: A qualitative meta-synthesis. J Clin Nurs. 2018;27(1-2):e21-e38.
Related Items

Uppföljningsfrekvens vid ILD

Övervakning av ILD-progression: vilket test ska utföras och när?

